
Pharma invests heavily in sales teams, messaging and promotional content. But are those efforts actually shifting prescribing behaviour and really moving doctors where it counts?
In our 2025 So What? Research Survey of 400+ Australian doctors, we asked what matters when it comes to treatment decisions and real-world prescribing, including:
Not all evidence carries equal weight, and not every tactic changes prescribing behaviour.
Here’s what we found.
We asked doctors what types of data they find most helpful when making treatment decisions. Their answers were clear.

Long-term follow-up data was ranked ‘very helpful’ by 49% of respondents making it the most trusted form of evidence. Doctors want proof that a treatment works not just in the short term, but over time.
Head-to-head trials ranked second (42%), valued for offering direct, comparative evidence.
“Just do head-to-head comparisons with proper backed research & data analysis and let doctors decide after that.” - General Practitioner
Clinical trials are also core to clinical thinking, with 41% ranking them ‘very helpful’, a figure that jumped to 79% among cardiologists.
“Positive data from well-designed clinical trials is THE best-selling point for any product.” - Haematologist
Global real-world evidence (35%) and systematic meta-analyses (34%) also performed strongly, especially among those seeking more comprehensive and credible insights.
“That trial data does not always translate to what the best therapy is for our individual patients. I am keen to see real world post marketing data.” - Rheumatologist
Patient case studies from peers were seen as the least helpful source. While relatable, only 13% of doctors found them ‘very helpful’ and nearly a third found them ‘unhelpful’.
Doctors want proof, not promotion. Long-term outcomes, robust comparisons, and real-world performance matter more than anecdotes or abstracts.
Beyond the clinical data, we also asked doctors what influences their prescribing. Their answers reveal what matters in practice, not just in theory.
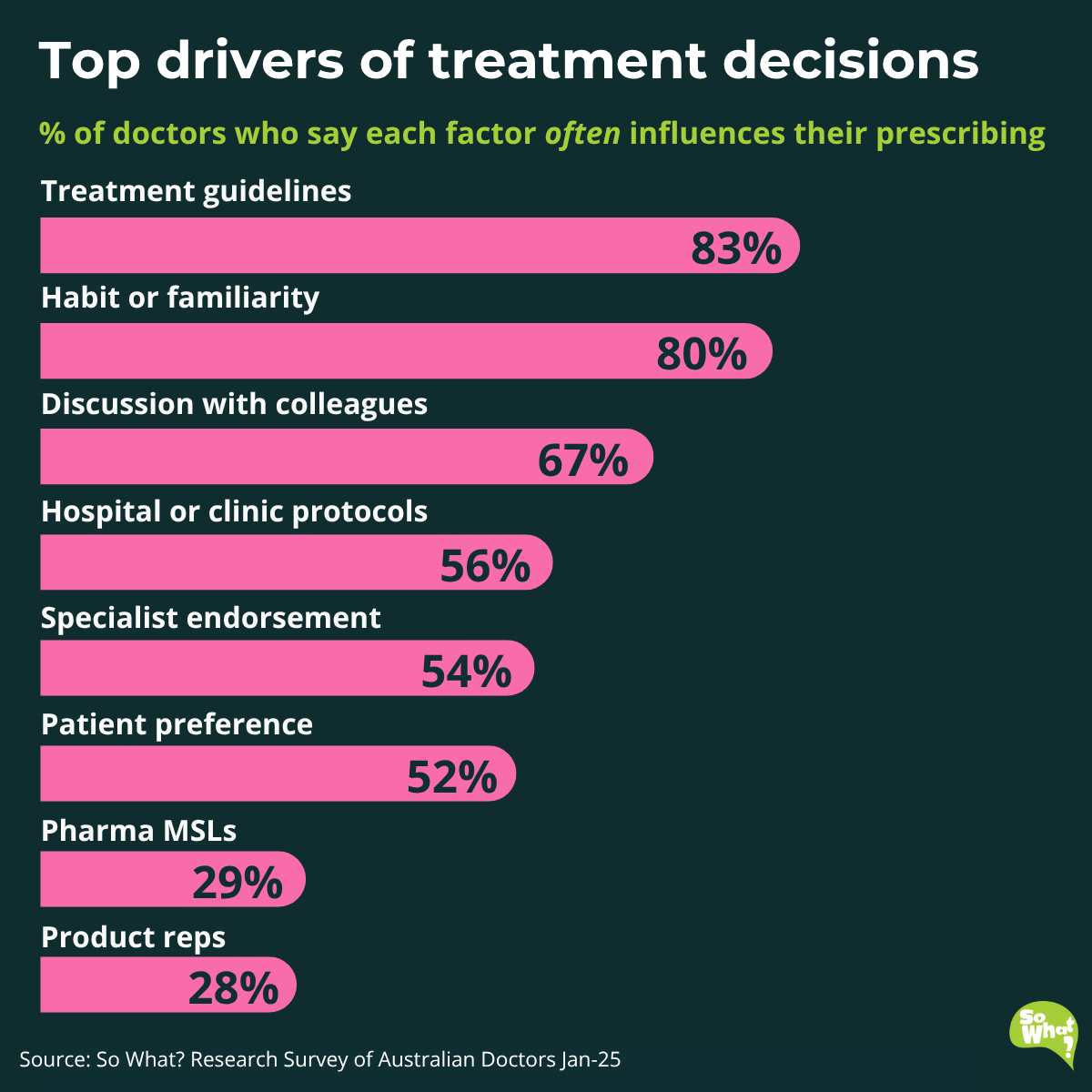
Clinical guidelines topped the list, influencing decisions for 83% of doctors. These provide a trusted framework, especially valuable in complex or fast-changing fields.
Habit and familiarity came next (80%), This reveals a key challenge as many doctors stick with what they know. Changing that requires strong, proven advantages.
Peer discussion (67%) is also influential. Doctors trust insights from colleagues, even when shared informally. Structured peer learning sessions is an opportunity for pharma to add value.
“More face to face educational meetings. A valuable way to learn from peers and specialist which are interactive.” - General Practitioner
Hospital protocols (56%) and specialist endorsements (54%) provide doctors with added structure and reassurance. These are particularly useful when treating outside their primary specialty.
Patient preference (52%) was selected by half the sample, highlighting the rise of shared decision-making. However, practical barriers like cost and complexity still limit how much sway it has in practice.
“It's always a shared decision making between me and my patients.” - General Practitioner
While MSLs (29%) and reps (28%) still play a role, their input only holds weight when it is precise, evidence-based, and clearly non-promotional. Doctors are quick to tune out anything that feels like a sales pitch.
“Pharma reps should stop forcing their product and just state the clear facts and studies. Visits should be about giving us information, then we choose to prescribe it or not. Stop making it a sales pitch.” - General Practitioner
Doctors are creatures of logic and habit. Influencing their decisions means backing your brand with quality evidence, structure, and relevance, not just repetition.
It’s not just what you share. It’s how you deliver it. We asked doctors which formats they prefer for receiving pharma updates, both in-person and digital, and their preferences were clear.
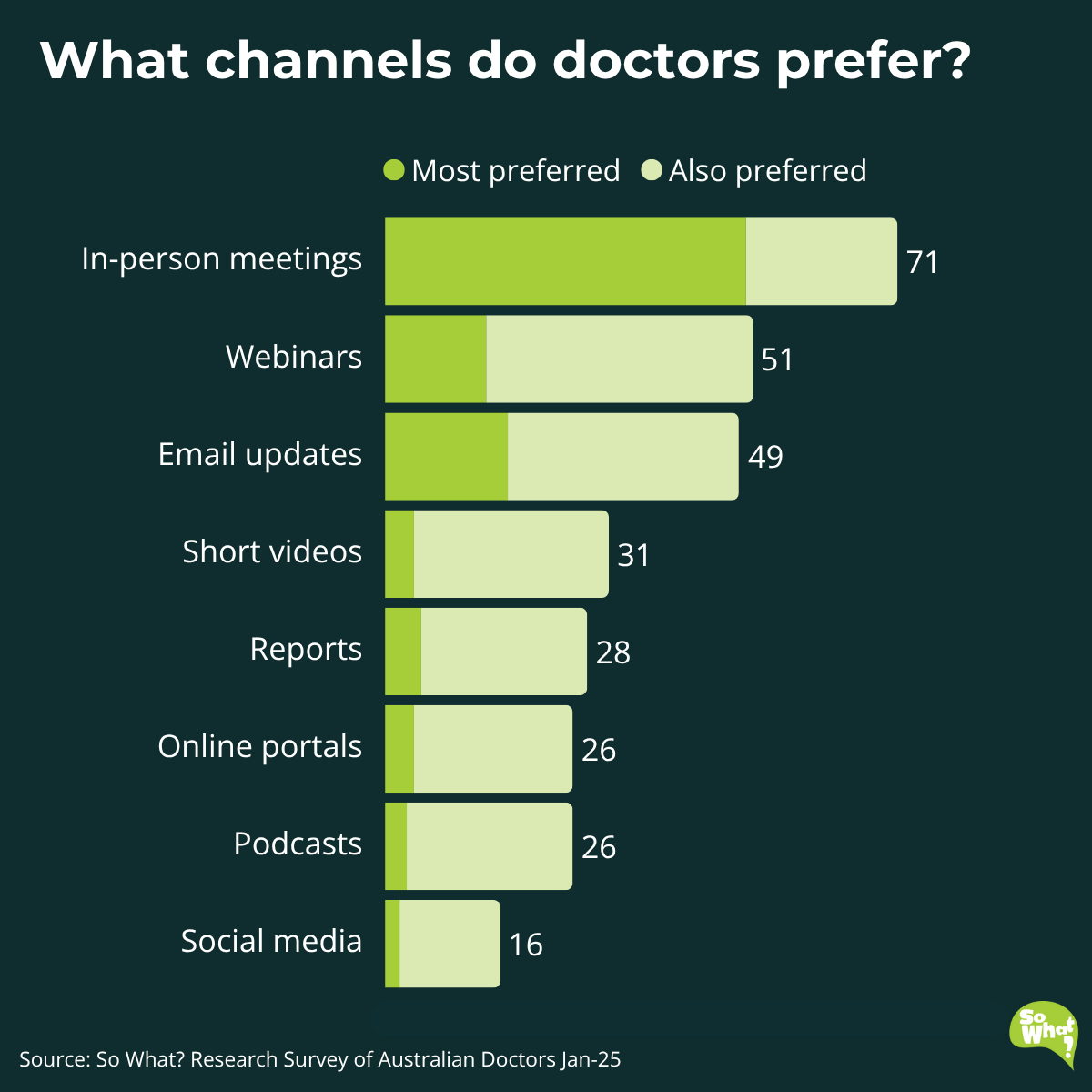
In-person meetings came out on top, by a wide margin. 71% of doctors said they prefer this channel, with 50% selecting it as their number one choice. Even with the rise of digital options, face-to-face interactions are still seen as the gold standard for engagement.
But digital channels are still important. Webinars (51%) and email updates (49%) were also highly rated, especially when time or geography makes in-person access difficult. Short videos and reports offer further opportunities, while social media ranked lowest.
These findings show how important it is to meet doctors where they are, both physically and digitally, and to choose communication formats that support the message.
Doctors have told us what they trust, how they decide, and how they want to be engaged.
The takeaway is clear: to influence prescribing where it matters, pharma needs to move from high-volume promotion to high-value support.
Here’s what that looks like in practice:

Doctors’ treatment decisions aren’t swayed by polished messaging. They’re grounded in trust, quality evidence, and delivery that fits the way they work.
That includes how the information is delivered. In-person meetings remain the gold standard for engagement, reinforcing the importance of personal, meaningful interaction.
Pharma’s role is to meet them there, with data and support that inform decisions, not just promote products.
We help pharma teams understand what doctors value and where your brand really stands.
Whether you’re planning a launch, refining engagement, or reshaping your message, we help you move beyond assumptions and closer to the moment decisions are made.
From evidence to execution, we turn insight into action, so you can make a stronger impact where it counts. Contact us today.